What are the molecular, cellular, and self-organizational principles that separate regeneration from fibrotic wound healing?
|
Animal development is breathtaking process whereby a single cell gives rise to all of the body's specialized cells and tissues. How would you reverse engineer this process to re-create tissue if it's lost or damaged?
That's exactly what happens during limb regeneration in salamanders - an assortment of complex tissues must produce and organize progenitors to re-develop lost structures. What makes this even more impressive is that unlike the embryo, that has a stereotypical limb size, regenerative processes are robust enough to adapt to changes in the size and position of the missing limb piece. Our primary research aim is to understand how cell intrinsic and extrinsic signals orchestrate cells and tissue to perfectly reconstruct the missing limb segments. |
Cell recruitment during regeneration
|
GFP-positive axolotl connective tissue cells "healing" a wound in culture |
One of the key events of regeneration is the formation of a proliferative mass of progenitors called the blastema. The blastema is the hallmark of nearly all animal regeneration, from worm heads to mouse fingertips. One of the key steps in forming the blastema is recruiting cells to migrate out of the stump tissue to the site of amputation. I found that the active migration of cells is critical for forming the blastema, and rather than one single wave of migration, cells are continuously migrating into the regenerating limb. The distance that cells migrate to contribute to the blastema also increases when a full limb needs to be regrown rather than a fingertip. Through in vitro and in vivo assays, I found that platlet-derived growth factor B (PDGFB) activates mesenchymal cells to migrate into the forming blastema. We are interested in how morphogens like PDGFB are modulated in space and time to control the source zone of migrating cells when different sized appendages need to be remade.
|
Coordinating cells in space and time
In addition to knowing how individual morphogens are regulated, we are interested in understanding how cell heterogeneity and spatial arrangement are used to build the blastema. Regeneration is triggered by amputation that can result in an arbitrary starting point anywhere along the limb. Despite this, the correct complement of progenitor cells are recruited and maintained in order to regrow exactly the missing segments. We want to know how blastema formation adapts to different starting positions and how the recruitment and proliferation of blastema progenitors is coordinated to create just the right amount of cells. We want to know what morphogenetic principles allow such adaptable organ building.
Deconstructing the process of making a blastema cell
One of the most enduring questions regarding regeneration is how do cells revert or "dedifferentiate" to a progenitor state that is sufficient to undergo re-development of the limb? We want to deconstruct the process of blastema cell formation to a set of extrinsic microenvironment signals (extracellular microenvironment) and intrinsic properties (gene expression profiles) that are sufficient to create and maintain limb progenitors. Our approach is to harness powerful ex vivo methods coupled with high spatio-temporal imaging to uncover instructive signals for dedifferentiation and how they are controlled in space and time.
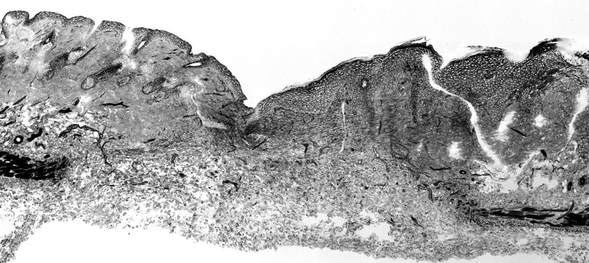
Making the leap: Identifying regenerative pathways and cell populations in scar-forming mammals
|
The goal of our work is to identify key steps that divert regenerative healing toward fibrotic scarring. There are clues that regenerative potential can be elicited in mammals. Mesenchymal stem cells have multipotent lineage potential in vitro, and in limited contexts mice and humans can regenerate the distal digit tip. Our working hypothesis is that adult, mammalian connective tissue fibroblasts (CTFs) exist which are intrinsically capable of responding regeneratively but are either 1) a small minority of total CTFs, 2) are diverted toward scarring by other signals, or 3) do not receive regenerative signals.
|
To test these possibilities, we use complimentary in vivo and ex vivo assays in the predominantly scar-forming mouse. This gives us the power to examine a complex wound environment that cannot be fully replicated in culture, while ex vivo assays allow us to challenge CTFs in isolation from potential scarring signals. As we identify subpopulations of regenerative cells in the mouse, and signals that push cells towards either scarring or regeneration, we will examine if the same mechanisms are conserved in humans.
By understanding the cellular and tissue-levels decisions that define regeneration in the axolotl, we are working toward improving the outcome of wound healing and regeneration in humans.
By understanding the cellular and tissue-levels decisions that define regeneration in the axolotl, we are working toward improving the outcome of wound healing and regeneration in humans.